NuPhy Halo 65 manuals are readily available online, offering comprehensive guidance for users across multiple languages. These resources detail setup,
customization, and troubleshooting for this popular mechanical keyboard.
Overview of the NuPhy Halo 65 Keyboard
The NuPhy Halo 65 is a compact 65% wireless mechanical keyboard celebrated for its aesthetic design and customizable features. Numerous online manuals, like those found on manuals.plus, provide detailed insights into its functionality. It boasts a gasket-mounted design for a unique typing experience and full-key hot-swappability, allowing users to easily change switches.
These manuals highlight the keyboard’s compatibility with various operating systems and its dual connectivity options – Bluetooth and USB-C. The Halo 65 aims to deliver a premium, customizable experience for both gamers and typists, with extensive RGB lighting options detailed in user guides;
Key Features and Specifications
NuPhy Halo 65 manuals detail key specifications, including its 65% layout, gasket mount, and hot-swappable switches. Available switch types vary, impacting the typing feel. Connectivity options encompass Bluetooth and USB-C, with Bluetooth version details found in the manuals.
The keyboard features customizable RGB lighting, controlled via software. Dimensions and weight are specified, aiding portability considerations. Manuals also cover battery life and charging information. The Halo 65 prioritizes customization, build quality, and a comfortable typing experience, as outlined in user documentation.

Setting Up Your NuPhy Halo 65
NuPhy Halo 65 manuals guide users through unboxing, connecting via Bluetooth or USB-C, and initial inspection for a seamless setup experience.
Unboxing and Initial Inspection
Upon receiving your NuPhy Halo 65, carefully examine the packaging for any signs of damage during transit. The box should contain the keyboard itself, a USB-C cable for wired connectivity, keycap puller, switch puller, and the user manual.
Inspect the keyboard thoroughly for any physical defects, such as scratches or dents. Verify that all components are present and in good condition. The manual provides a detailed inventory list. Retain the original packaging for potential warranty claims or returns. A quick visual check ensures a positive initial experience.
Connecting via Bluetooth
To connect your NuPhy Halo 65 via Bluetooth, first, ensure the keyboard is powered on. Press and hold the Bluetooth pairing button – typically located on the keyboard’s side or back – until the indicator light begins flashing.
On your device, navigate to Bluetooth settings and search for available devices. Select “NuPhy Halo65” from the list. Follow any on-screen prompts to complete the pairing process. The indicator light will become solid once connected. Refer to the manual for specific button locations.
Connecting via USB-C
Connecting your NuPhy Halo 65 via USB-C is straightforward. Simply plug the included USB-C cable into the keyboard’s USB-C port and connect the other end to a compatible USB port on your computer or device.
The keyboard should be recognized automatically, requiring no additional driver installation in most cases. This method provides a stable, low-latency connection ideal for gaming or tasks demanding precise input. The manual confirms this plug-and-play functionality for seamless operation.

Understanding the Keyboard Layout
The NuPhy Halo 65’s layout is a compact 65% design, balancing functionality and portability. Manuals detail key placements, function layer access, and dedicated media controls.
Keycap Overview and Materials
The NuPhy Halo 65 typically features double-shot PBT keycaps, renowned for their durability and resistance to shine. Manuals highlight the benefits of PBT over ABS plastic, emphasizing longevity and texture. These keycaps are designed to withstand extensive use, maintaining their appearance and feel over time.
The double-shot molding process ensures legends won’t fade, as the plastic is molded in two separate stages. User guides often illustrate how to carefully remove and replace keycaps for cleaning or customization, offering guidance on compatible keycap profiles and materials for optimal performance.
Function Layer Access
The NuPhy Halo 65 utilizes a function (Fn) key to access secondary functions printed on certain keycaps. Manuals detail how pressing Fn in combination with other keys activates features like media controls, volume adjustment, and navigation; Customization software allows remapping these functions to suit individual preferences.
Users can access multiple function layers, expanding the keyboard’s capabilities beyond standard inputs. Guides illustrate the default Fn key assignments and explain how to modify them through the NuPhy software, providing a tailored user experience and increased productivity.
Dedicated Media Controls
The NuPhy Halo 65, as outlined in its manuals, features dedicated media controls accessible via the function layer. These controls allow for convenient playback, pause, skip, and volume adjustment without interrupting workflow. Users can easily manage their audio experience directly from the keyboard.
The manual details specific key combinations for each media function, ensuring quick and intuitive operation. Customization software further enhances control, enabling remapping of these keys to preferred functions or macros, tailoring the keyboard to individual media consumption habits.

Customization Options
NuPhy Halo 65 manuals highlight extensive customization, including software installation, key remapping, macro programming, and vibrant RGB lighting effects configuration.
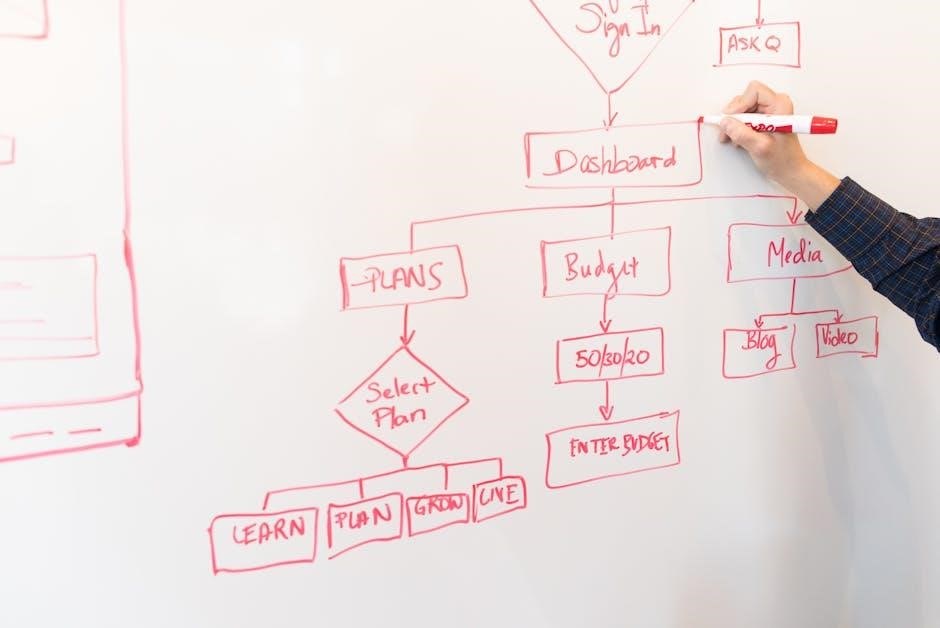
Software Installation and Overview
The NuPhy Halo 65 requires dedicated software for full customization. Manuals detail downloading and installing the NuPhy Console, compatible with Windows and macOS.
This software provides a user-friendly interface to modify key assignments, program macros, and control the keyboard’s sophisticated RGB lighting. The overview within the manual explains each section of the software, guiding users through the process of tailoring the keyboard to their preferences.
It also covers firmware updates, ensuring optimal performance and access to new features.
Key Remapping and Macro Programming
NuPhy Halo 65 manuals thoroughly explain key remapping within the NuPhy Console software. Users can redefine any key’s function, optimizing the layout for specific applications or workflows.
Macro programming allows recording and assigning complex sequences of keystrokes to a single key. This feature significantly boosts efficiency for repetitive tasks. The manual provides step-by-step instructions, including how to save, load, and manage custom macros.
Detailed examples illustrate the process, making it accessible for all skill levels.
RGB Lighting Effects Configuration
NuPhy Halo 65 manuals dedicate a section to customizing the keyboard’s vibrant RGB lighting. The NuPhy Console software offers extensive control over colors, patterns, and brightness. Users can select from pre-set effects like static, breathing, or wave, or create entirely custom lighting schemes.
The manual details how to adjust speed, direction, and color palettes. It also explains synchronization options, allowing the lighting to react to keystrokes or music.
Detailed screenshots guide users through the software interface.
Advanced Features
NuPhy Halo 65 manuals explain wireless and wired modes, battery management, and charging procedures. These features enhance usability and customization options for users.
Wireless Mode Operation
NuPhy Halo 65 manuals detail a straightforward Bluetooth connection process, enabling seamless wireless operation. Users can connect to multiple devices and easily switch between them. The manual emphasizes the keyboard’s stable wireless performance and extended range, offering freedom from cable clutter.
It also provides guidance on optimizing battery life in wireless mode, including tips for managing RGB lighting and utilizing power-saving features. Troubleshooting steps for connectivity issues are clearly outlined, ensuring a smooth wireless experience. The manual highlights the convenience and versatility of the Halo 65’s wireless capabilities.
Wired Mode Operation
NuPhy Halo 65 manuals explain that connecting via USB-C provides a stable, low-latency wired connection, ideal for gaming or tasks demanding precise input. The manual details the simple plug-and-play setup, requiring no additional drivers for most operating systems.
It clarifies that wired mode bypasses battery usage, offering uninterrupted operation. Troubleshooting steps address potential USB connectivity issues, ensuring a reliable connection. The manual also notes that certain customization features might function differently in wired mode compared to wireless, offering a comprehensive understanding of both modes.
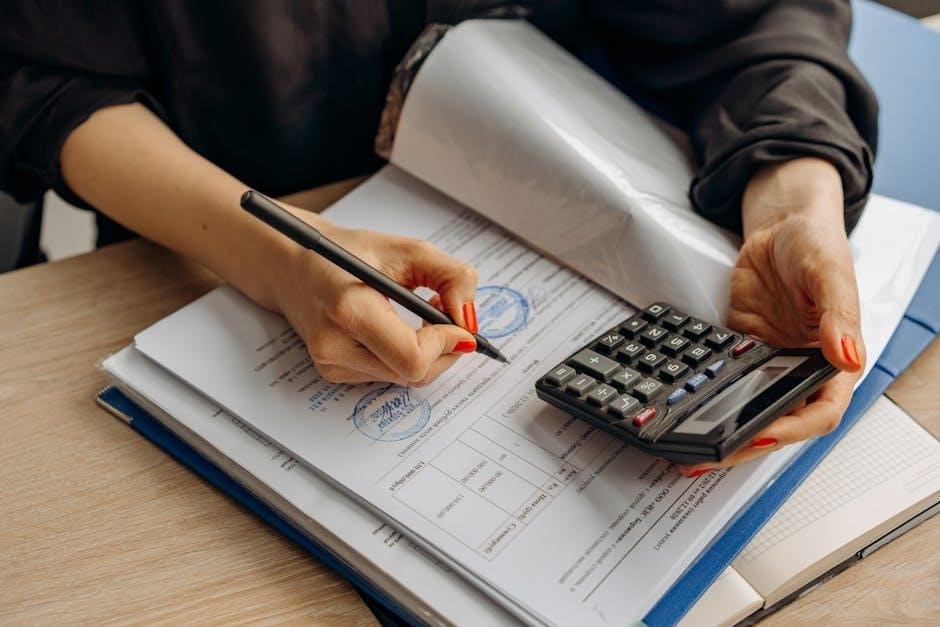
Battery Management and Charging
NuPhy Halo 65 manuals detail the keyboard’s battery life, typically lasting for extended use depending on RGB settings and usage intensity. The manual emphasizes using the provided USB-C cable for optimal charging. It advises against using fast chargers, as they may impact battery health.
The manual explains how to check the battery level via software or keyboard indicators. It also provides guidance on maximizing battery life, such as adjusting RGB brightness and utilizing sleep mode. Troubleshooting steps address scenarios where the keyboard fails to charge or hold a charge.

Troubleshooting
NuPhy Halo 65 manuals offer solutions for common issues like connectivity problems, keycap malfunctions, and software conflicts, ensuring smooth operation.
Connectivity Issues
If experiencing Bluetooth connection problems with your NuPhy Halo 65, the manual suggests first ensuring the keyboard is sufficiently charged. Attempt re-pairing the device within your operating system’s Bluetooth settings.
For USB-C connectivity failures, verify the cable is securely connected to both the keyboard and your computer. Try a different USB-C port or cable to rule out hardware issues. The manual also advises checking for driver updates if using a Windows system, as outdated drivers can sometimes cause connectivity disruptions.
Interference from other wireless devices can also impact Bluetooth stability; try moving away from potential sources of interference.
Keycap Problems
The NuPhy Halo 65 manual details keycap removal and replacement procedures. If a keycap becomes loose or detached, gently use a keycap puller to remove it, avoiding excessive force. Ensure the stem is undamaged before reattaching.
For issues with keycap legends fading or wearing off, the manual doesn’t offer repair solutions, as this is considered normal wear and tear. However, it highlights the availability of replacement keycap sets from NuPhy and third-party vendors.
If a keycap is broken, immediate replacement is recommended to prevent damage to the switch underneath.
Software Conflicts
The NuPhy Halo 65 manual addresses potential software conflicts arising from simultaneous operation of multiple keyboard customization programs. It advises closing other similar software before launching the NuPhy software to ensure proper functionality.
Conflicts with system-level hotkey managers can sometimes occur, causing remapped keys to behave unexpectedly. The manual suggests temporarily disabling such managers to isolate the issue and verify NuPhy software control.
If conflicts persist, a clean reinstall of the NuPhy software is recommended, following the instructions provided in the manual.

Maintenance and Care
The NuPhy Halo 65 manual details cleaning instructions, keycap replacement guidance, and procedures for essential firmware updates to maintain peak performance.
Cleaning Instructions
Maintaining your NuPhy Halo 65 is straightforward. The official manual recommends disconnecting the keyboard before cleaning. Use a soft, dry cloth to wipe down the keycaps and chassis regularly, removing dust and debris. For stubborn marks, lightly dampen the cloth with water – avoiding excessive moisture.
Do not use harsh chemicals or abrasive cleaners, as these can damage the keycaps or finish. For deeper cleaning, keycaps can be carefully removed using a keycap puller (not included) and washed with mild soap and water, ensuring they are completely dry before reattaching.
Keycap Replacement
Replacing keycaps on your NuPhy Halo 65 allows for personalization. A keycap puller (sold separately) is essential to avoid damage. Gently and evenly pull upwards on the keycap, avoiding excessive force. Ensure replacement keycaps are compatible with the Halo 65’s switches – typically MX-style switches.
When reinstalling, align the stem of the new keycap with the switch and press down firmly until securely seated. Be cautious not to damage the switch pins during removal or installation. Explore custom keycap sets to enhance your keyboard’s aesthetic!
Firmware Updates
Keeping your NuPhy Halo 65’s firmware updated ensures optimal performance and access to the latest features. Download the latest firmware from the official NuPhy website. The NuPhy software facilitates the update process; follow the on-screen instructions carefully.
During the update, avoid disconnecting the keyboard or interrupting power. A stable USB-C connection is crucial. Firmware updates can address bugs, improve compatibility, and introduce new functionalities. Regularly check for updates to maintain a smooth user experience.

Specific Key Functions
The NuPhy Halo 65 manual details specific key functions, including print screen shortcuts and multimedia controls, enhancing user efficiency and keyboard utility.
Print Screen Functionality
The NuPhy Halo 65 manual clarifies the print screen key’s operation. Often, it’s not a standard key and requires a function key combination. Users should consult the manual to determine the precise key sequence for capturing screenshots.
Typically, this involves holding down the ‘Fn’ key while pressing the designated print screen key. The manual will illustrate this combination visually. Some versions may offer full-screen capture or selective region capture options, further detailed within the documentation. Understanding this functionality streamlines content creation and sharing.
Volume Control Keys
The NuPhy Halo 65 manual details how to utilize dedicated volume control keys, often integrated with function key presses. Typically, these keys – volume up, down, and mute – require holding the ‘Fn’ key simultaneously. The manual provides a clear diagram illustrating the key locations and corresponding functions.
Users can quickly adjust audio levels without interrupting their workflow. Precise key combinations are outlined, ensuring seamless control over system volume. The manual also clarifies if these functions are customizable through the NuPhy software.
Multimedia Key Functions
The NuPhy Halo 65 manual comprehensively explains the keyboard’s multimedia key functions, often accessed via the ‘Fn’ key layer. These controls typically include play/pause, skip forward, skip backward, and potentially stop functions for media playback. The manual visually maps these functions to specific key combinations.
Users can effortlessly manage their music and videos without switching applications. Detailed instructions ensure easy navigation through playlists and media controls. Customization options within the NuPhy software may allow remapping these functions to suit individual preferences.

Technical Specifications
The NuPhy Halo 65 manual details dimensions, weight, available switch types, and Bluetooth specifications. It provides precise technical data for informed user understanding.
Dimensions and Weight
According to the NuPhy Halo 65 manual, understanding the keyboard’s physical attributes is crucial for desk setup and portability. The Halo 65 boasts a compact 65% layout, measuring approximately 307.5mm x 104mm x 40mm (12.11in x 4.09in x 1.57in).
Its weight is around 1.83kg (4.03lbs), contributing to its stable feel during intense gaming or typing sessions. These specifications, detailed within the manual, help users assess compatibility with their workspace and travel needs, ensuring a comfortable and efficient experience.
Switch Types Available
The NuPhy Halo 65 manual highlights a diverse range of switch options to cater to varied user preferences. Available switches include NuPhy Halo Sky, Halo Pink, and Halo Peach, each offering distinct tactile feedback and actuation forces.
Additionally, compatibility with Cherry MX style switches allows for further customization. The manual details the characteristics of each switch, aiding users in selecting the optimal type for their typing style and gaming needs, ensuring a personalized and comfortable experience.
Bluetooth Version and Range
The NuPhy Halo 65 manual specifies the keyboard utilizes Bluetooth 5.0, ensuring a stable and efficient wireless connection. This version provides an extended range, typically up to 33 feet (10 meters) in open environments.
However, the manual notes that range can be affected by interference from other wireless devices or physical obstructions. It also details how to pair the keyboard with multiple devices and switch seamlessly between them, maximizing usability and convenience.

Safety Precautions
The NuPhy Halo 65 manual advises against disassembly and exposure to liquids. Always use a compatible USB-C charger to prevent electrical hazards.
General Usage Guidelines
The NuPhy Halo 65 manual emphasizes proper handling to ensure longevity. Avoid dropping or subjecting the keyboard to strong impacts, as this could damage internal components.
Keep the keyboard away from extreme temperatures and humidity. Regularly check the USB-C cable for fraying or damage, and replace if necessary.
When cleaning, disconnect the keyboard to prevent accidental key presses or electrical shock. Do not attempt to disassemble the device beyond keycap removal, as this will void the warranty.
Always refer to the manual for specific instructions regarding customization and advanced features.
Electrical Safety Information
The NuPhy Halo 65 manual stresses the importance of using a certified USB-C power adapter. Avoid using damaged cables or power sources, as this poses a risk of electrical shock or fire.
Do not expose the keyboard to water or other liquids, as this can cause short circuits.
Never attempt to repair the keyboard yourself; contact qualified personnel for assistance. Disconnect the keyboard from the power source before cleaning or performing maintenance.
Ensure the voltage of the power adapter matches your local electrical supply. Follow all local electrical safety regulations.

Warranty Information
NuPhy Halo 65 manuals detail warranty coverage, typically one year, against manufacturing defects. Contact NuPhy support to initiate a warranty claim, providing proof of purchase.
Warranty Coverage Details
NuPhy’s Halo 65 warranty generally covers defects in materials and workmanship under normal use for a period of one year from the original purchase date. This doesn’t include damage from misuse, accidents, modifications, or natural disasters.
The warranty specifically addresses issues like malfunctioning keys, PCB failures, or problems with the wireless connectivity. Cosmetic wear and tear, or keycap damage, are typically excluded. To be eligible, retain your original proof of purchase and contact NuPhy’s customer support for assistance.
How to Claim Warranty
To initiate a warranty claim for your NuPhy Halo 65, first contact NuPhy’s customer support team via their official website; You’ll need to provide your original proof of purchase, a detailed description of the issue, and potentially photos or videos demonstrating the defect.
NuPhy will then provide instructions, which may involve returning the keyboard for inspection. Shipping costs for the return may be the responsibility of the customer, depending on the specific case and warranty terms.